by Susan Gee, Tracey Hawkes and Julia Bergman
Download the full article for free.
Delirium is common amongst older people in hospital, but up to a third of new cases may be prevented by introducing simple preventative protocols. Addressing these preventable risk factors can seem like stating the obvious to staff: ‘But aren’t we doing that already?’ An AI approach provided a way to encourage staff to reflect and identify changes themselves. In a small-scale demonstration project, the AI process led to a significant improvement in awareness amongst the staff.
Delirium is a common and serious illness amongst older people in hospital, but it is be able to be prevented in many cases. An Appreciative Inquiry approach offered us a way to respectfully find out what was working well and how this could inform and inspire improvements in delirium prevention.
The context
Delirium is sudden confusion which develops over hours to days. People with a delirium have trouble thinking clearly, focusing their thoughts and paying attention. This tends to fluctuate across the course of the day. It is different from dementia, which is a progressive cognitive decline that develops and progresses over time. Delirium is under-recognised but surprisingly common, particularly among older people who are hospitalised. Delirium can have lasting and grave consequences for a patient’s recovery, with an increased risk of staying in hospital longer, having more complications, being discharged to long-term care, and dying. (National Institute for Health and Clinical Excellence, 2010).
The potential
A considerable proportion of delirium affecting older people in hospital develops after admission. These are the cases that we can often prevent with better care.
Anything that impacts on the brain can increase the risk of delirium. Conversely, anything that can be done to reduce a cause or risk factor could help prevent delirium. The focus is to target the triggers that can occur during the episode of care. There is considerable consensus about these preventable risk factors to guide prevention protocols. International evidence shows that new cases of delirium developing during admissions can be reduced by a third or more using interventions that target and reduce identified risk factors (Martinez, Tobar and Hill, 2015; Hshieh et al., 2015). Indeed there is more evidence to support the effectiveness of making changes to prevent delirium than there is to support making changes to better treat or manage delirium once it occurs (Francis, 2014).
The barrier
The components of these interventions are simple but the key is consistency. Despite the knowledge that delirium can be reduced, hospitals are indeed in a persistent “know-do” gap:
… as the evidence grows, the state of implementation is not keeping up … Why, then, are these protocols not more widely implemented? … there may be an assumption held by many physicians and hospital leaders along the lines of “aren’t we doing all this stuff already?” Perhaps because most of the interventions to reduce delirium are protocol-based and nursing-driven, it may be easy to assume that such measures are already in place and running in the background at many hospitals. Numerous components of these interventions may simply seem too simple to question that they are not being done already. (Greyson, 2015, p. 521).
In previous studies, the push to change practice to a more preventative approach was supported by a considerable investment of resources in the form of a designated position and/ or a team of volunteers. In the absence of these types of resources, the gap between the potential and actual practice remains.
The AI fit
It seemed to us that an AI approach offered a powerful way to overcome the “but aren’t we doing that already” hurdle, to encourage staff to reflect and identify changes themselves. AI shares many of the values of nursing and allied health professions, and provides an approach that is supportive and respectful (Reed, 2010). Rather than raising defensiveness by a problem-focused or didactic approach, AI recognises the health professionals involved as experts in their own experience who have much to offer, with specialised skills and knowledge that we can access and utilise (Reed, 2010).
Reflective practice is a key skill for nursing and allied health professionals. Natius Oelofsen (2012) discusses how reflective practice starts with curiosity about a puzzling situation and hopefully concludes with a sense of clarity and understanding. This is achieved through a process of looking closer and finding new ways of answering the questions that were raised. AI can be seen as scaffolding health professionals’ self-reflection and providing a way to focus on how best practice can be maintained and further developed (Bellinger & Elliot, 2011; Stefaniak, 2007). The group nature of AI enables conversations that help health professionals to focus on and strengthen their skills and positive experiences, but also to imagine possibilities together that may go beyond what any one individual might create themselves (Wasserman and Namee, 2010).
The project
The participants were recruited through invitations at Older Person’s Health Specialist Service education days and learning networks. The fifteen volunteers were spread amongst various wards and outpatient teams and twelve nurses, a social worker, an occupational therapist and a physiotherapist.
A key feature of an AI approach is that the methods of inquiry are themselves part of the intervention. Inquiry and change are simultaneous and, by stimulating reflection, inquiry can lead to different ways of thinking (Reed 2007, 2010). To document this we introduced a repeated measures design: a baseline individual interview, a guided AI group discussion, and then a follow-up individual interview.
While an AI discovery phase often begins with the participants interviewing each other, we began with a separate one-to-one interview with a member of the research team. This interview began the appreciative discovery process by framing the conversation with positive questions, but also provided a baseline measure of awareness of the status of risk factors in day-to-day practice. The interviewer asked participants to think about the last older patient in their case load that they interacted with. The preventable risk factors were simplified by a PINCHES ME Kindly mnemonic: Pain, Infection, Nutrition and Constipation, Hydration, Exercise, Sleep, Medication, Environment and person-centred care (kindly). The discussion went through each of the risk factors in turn, for example “Was Mr X in pain? How did you know?” We also asked participants to talk about what was working well to help to prevent, identify or manage each risk.
We gathered the participants together into small groups for a guided AI discussion or “brainstorming session” with the research team. The brain storm was semi-structured to lead the discussion through an iteration of the AI cycle, but remain flexible and fluid (Reed, 2007). The core questions that guided the discussion (see Table 1) opened with sharing what participants were proud of, and flowed on to how things could be even better, and the steps that could be taken to get there. Again, we used the PINCHES ME Kindly mnemonic to help collate the tips and ideas during the discussion about what people were proud of and the magic wand question, with a large sheet of paper for each risk factor alongside broader environmental factors.
Follow-up interviews a month later allowed us to gauge how much had changed since the first interview and what the participants thought of the process. Staff were again asked to talk individually about a specific case to provide a post-intervention measure of awareness of risk factors.
To document the impact of the reflective process on the individuals involved, the awareness of risk factors from each interviews was categorised as 1: cursory, 2: moderate, or 3: thorough by each of the three researchers. The coding was then compared and any discrepancies resolved by consensus, with evolving coding notes to clarify future decisions.
To help embed and sustain change, specific projects that emerged from the discussion were dovetailed into the work stream of the existing Dementia and Delirium group. A link group was set up to enable participants and other interested staff to remain involved.
|
Phase |
Key questions / activities |
|
Discovery Sharing the positive |
One-to-one interviews: What is working well…? Group, opening question: You’ve all had the opportunity to reflect about what’s happening with delirium prevention for you currently, and we’d like to start by gathering together some ideas about what is being successful. Thinking back about your interviews – what parts made you feel proud to talk to share. What’s working well for you for delirium prevention? |
|
Dream Sharing a vision |
Group, magic wand question: … We’ve gathered together some of the good things that you are doing that really work for delirium prevention. How might we make it better? If you could transform the way you work so that you are more focused on delirium prevention, what would it look like, what would it take to happen? Imagine that you can wave your magic wand and anything is possible – for you, your team, your environment. You’ve got three wishes for delirium prevention in your own work setting – what are they going to be? |
|
Design Sharing what we think should be |
Group, developing provocative propositions (Bridging dream and design): We are going to come up with some statements – our vision, our goal for what we are going to look like in a couple of years when we “think delirium” in our work setting. They are going to be positive. And they going to be bold: “if you are good we want better, if you are great we want outstanding…” Group: Identifying specific “projects” for the service that would make a difference |
|
Delivery Sharing a commitment to change |
Group, personal goals: Now our last thing is that we want you to think about your own goals in the short term. We’ve got a sheet here for you to fill in three goals – what are you are to aim to do when you walk out that door? One-to-one follow-up interview Action planning and implementation: Specific projects were followed through with the support of delirium groups and the participants could remain involved through a link group Six-month survey |
The actions
Part of the Appreciative Inquiry process is to take the ideas that have been generated about what is working and visions for the future, and to turn them into concrete actions about what could be done differently. The AI process was an effective kick-starter for sparking a number of further specific projects.
The vision for a service that “thinks delirium prevention” that emerged had three overarching themes: committed, consistent and a great care environment. We used the simple PINCHES ME Kindly mnemonic to summarise risk factors during the project. The participants strongly embraced this and wanted it to be the core of the ongoing actions.
A committed environment included being proactive about delirium prevention with PINCHES ME Kindly ingrained throughout the service. Identified actions included education, reminders and resources to encourage this.
Collating the Discovery and Dream phase questions can be seen as forming the basis of a good practice guide (Bellinger and Elliott, 2011). A user-friendly fun booklet was created to share the tips and possibilities from participants to inspire other staff (Gee, Bergman, Hawkes & Croucher, 2016). This well-received book provides a useful bridge between abstract international guidelines and how they can be operationalised in daily practice.
- A poster/handout summary version of PINCHES ME Kindly was created for publicity and education.
- The THINKdelirium resources are being used by CDHB nurses in orientation and in-house education, and there are moves to spread this, given that delirium prevention requires a multidisciplinary approach. A multidisciplinary working group has been set up to integrate the THINKdelirium booklet into an online education package.
- An annual “Spring Into Delirium” day has been initiated to raise awareness of the THINKdelirium messages and resources and where to locate them.
- The consistent theme focused on consistently and comprehensively assessing and addressing the risk factors. Identified actions included having documentation resources available to accurately monitor relevant risk factors.
- A THINKdelirium webpage has been created on the staff intranet. This provides an interactive summary of PINCHES ME Kindly, with links to download the THINKdelirium and associated documentation resources.
- A summary of the PINCHES ME Kindly message has been added to the routine documentation for hospital aids when they are providing close observation.
- Staff are considering how the PINCHES ME Kindly message can be included in records and discharge documentation.
- A great care environment focused on providing person-centred care. Identified actions included more resources for activities, and a prevention-focused brochure for care-partners.
- The staff were keen to be supported to encourage meaningful activity for older people on the wards. A follow-up project is trialling the introduction of “activity trolleys” with activity resources and tips alongside a staff-education package.
- Staff wanted ways to engage care partners to help prevent older people getting delirium. Based on international exemplars, a prevention-focused brochure for those supporting older people in hospital has been developed.
The impact for participants
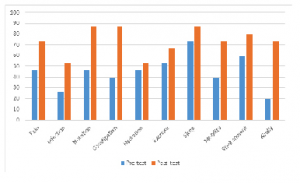
The AI approach was effective in engaging staff and overcoming the “aren’t we doing that already” hurdle. A nonparametric Wilcoxon signed-rank test was used to test the difference between the sum pre-test and post-test scores, and an effect size was calculated (Field, 2009). There was a significant improvement in the awareness of the status of the target risk factors for older people in their care when the follow-up interviews were compared with the baseline interviews (z = 3.21, p. <.001,) with a moderate effect size of .59. This change is illustrated in Figure 1 which shows the increase in the proportion of the participants being given the highest rating of awareness for each of the risk factors.
All of the participants gave positive qualitative feedback about being involved in the project during the follow-up interviews, with the predominant themes being that they “enjoyed the process”, and “learned a lot”. A six-month follow-up survey was completed by fourteen of the fifteen participants, and again all were positive about the project. In particular, all the participants agreed that the project inspired them to do more to pro-actively prevent delirium, and that it was worthwhile taking part in the project. Twelve of the respondents identified specific changes in their personal practice and thirteen identified activities or changes that they were inspired to champion in their workplace.
Examples of feedback included
Everyone on our ward has thought the booklet is fantastic. We have found it really useful for our nursing students also. We also love the brochure for families … What a fantastic project to be involved in! It challenged my thinking and made me think about my practice.
My awareness of delirium [now] makes me ask more specific questions regarding risk factors in my assessments. I also provide information/education to clients/families where appropriate. I have provided an in-service session to my immediate team … and [plan to] discuss with the team to include [delirium tool] in our initial assessment tools. I very much appreciated being able to participate in the project.
The discussion
There are well-established guidelines for delirium prevention (e.g., National Institute for Health and Clinical Excellence, 2010), with good evidence of the benefits when they are followed (Martinez, Tobar and Hill, 2015; Hshieh et al., 2015). However, while guidelines are commonly produced as a tool to promote best practice, it has been recognised that on their own they often have little impact on behaviour (Greyson, 2015) and that strength of evidence is not a good predictor of the likelihood of adherence (Ricart et al., 2003). AI was a very effective tool to help to bridge the gap between the abstract guidelines (but aren’t we doing that already?) and what that could look like in the real world. AI gave a way of basing our projects and resources on listening, which has helped to increase engagement and ownership. While we have not yet achieved our ideal vision for the organisation we are excited about the collaborative steps we are taking toward it.
We were drawn to the AI approach for this project because of our positive experiences using an AI approach with our adult students, and our recognition of the synergy between an AI approach and reflective professional practice. Appreciative Inquiry holds that at its best, change is a process of inquiry grounded in affirmation and appreciation (Whitney and Trosten-Bloom, 2010). The AI approach was a chance to provide recognition of the staff and help them work from their strengths (Whitney and Trosten-Bloom, 2010). The staff were respected as experienced professionals, and their contributions were recognised and valued as a resource to be shared. The approach encouraged the participants to recognise the importance of what they do and their potential to make a difference. The AI approach was about asking questions, not providing solutions.
Reflective practice itself can be seen as a process of inquiry: the process of asking questions helps us to look at what we are doing and reflect on how we can do things even better. The use of positive questions and constructing positive images of the future in the AI process helped to inspire positive change. The AI process worked so well because it was both visionary and pragmatic. It helped to inspire a larger vision of an ideal environment while also exploring the small practical steps that could be taken (Loveday, 2011). The AI process was not just a constructive process for generating actions for the teams, but also a positive and effective learning experience for the individual participants.
References
Bellinger, A. and Elliott, T. (2011) What are You Looking At? The potential of Appreciative Inquiry as a research approach for social work, British Journal of Social Work, 41, 708–725.
doi: http://dx.doi.org/10.1093/bjsw/bcr065
Kadi-Hanifi, K., O. Dagman, J. Peters, E. Snell, C. Tutton, and T. Wright. (2014) Engaging Students and Staff with Educational Development Through Appreciative Inquiry, Innovations in Educational and Teaching International, 51(6), 584–594.
doi: http://dx.doi.org/10.1080/14703297.2013.796719
Field, A. (2009) Discovering Statistics Using SPSS (3rd Ed.). London, UK: Sage.
Francis, J. (2014) Delirium and Confusional States: Prevention, treatment, and prognosis. In M. J. Aminoff and K. E. Schmader, (Eds), UpToDate, Waltham, MA: Wolters Kluwer Health.
Gee, S., J. Bergmann, T. Hawkes and M. Croucher. (2016) THINKdelirium Preventing Delirium Amongst Older People in Our Care. Tips and Strategies from the Older Persons’ Mental Health THINKDelirium Prevention Project. Christchurch, NZ: Canterbury District Health Board. Available from: www.cdhb.health.nz/delirium
Greyson, S. R., (2015) Delirium and the “Know-do” Gap in Acute Care for Elders, JAMA Internal Medicine, 175(4), 521–522.
Hshieh, T. T., J. Yue, E. Oh, M. Puelle, S. Dowal, T. Travison and S. K. Inouye. (2015) Effectiveness of Multicomponent Nonpharmacological Delirium Interventions: A meta-analysis, JAMA Internal Medicine, 175(4), 512–520.
doi: http://dx.doi.org/10.1001/jamainternmed.2014.7779
Loveday, B. (2011. Dementia Training in Care Homes. In T. Dening and A. Milne (Eds.) Mental Health and Care Homes (pp. 327–344). Oxford, UK: Oxford University Press.
Martinez, F., C. Tobar and N. Hill, N. (2015) Preventing Delirium: Should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature, Age and Ageing, 44(2), 196–204.
doi: http://dx.doi.org/10.1093/ageing/afu173
National Institute for Health and Clinical Excellence. (2010) Delirium: Diagnosis, prevention and management (Clinical guideline 103). London, UK: NICE. Available from www.nice.org.uk/CG103.
Oelofsen N. (2012) Using Reflective Practice in Frontline Nursing. Nursing Times, 108(24), 22–24.
Reed, J. (2007) Appreciative Inquiry: Research for Change. Thousand Oaks, CA: Sage.
Reed, J. (2010). Appreciative Inquiry and Older People–Finding the Literature. International Journal of Older People Nursing, 5(4), 292–298.
Ricart, M., C. Lorente, E. Diaz, M. H. Kollef and J. Rello. (2003) Nursing Adherence with Evidence-based Guidelines for Preventing Ventilator-associated Pneumonia, Critical Care Medicine, 31(11), 2693–2696.
doi: http://dx.doi.org/10.1097/01.CCM.0000094226.05094.AA
Stefaniak, K. (2007) Discovering Nursing Excellence through Appreciative Inquiry, Nurse Leader, 5(2), 42–46.
doi: http://dx.doi.org/10.1016/j.mnl.2007.01.010
Wasserman, I.C. and S. McNamee. (2010) Promoting Passionate Care with Older People: A relational imperative, International Journal of Older People Nursing, 5, 309–316.
Whitney, D. and A. Trosten-Bloom. (2010) The Power of Appreciative Inquiry (2nd Ed). San Fancisco, CA: Berrett-Koehler.